Providing optimal nutrition therapy to critically ill patients in the high technological environment of the ICU can be challenging. The Critical Care Nutrition resource center provides tools to facilitate implementation of nutrition guidelines. This page provides guidance on how to use these tools to improve nutrition practices.
1. Audit Your Nutrition Practice
By auditing your current nutrition practice and comparing your results to nutrition guidelines recommendations and to other ICUs, you can demonstrate your strengths and identify opportunities for improvement.
The EFFORT Trial is an initiative that assists you in auditing your practice by providing the necessary measurement tools and generating a benchmarked performance report.
2. Standardize Care
Nutrition therapy can be improved by standardizing the delivery of nutrition through the implementation of bed-side protocols such as pre-printed orders, algorithms, and care pathways. Evidence based protocols can help to automate the initiation of nutrition, reduce errors, and improve the quality of patient care.
Several examples of these bed-side tools are available in the Resource Center. These tools can be used as a template to develop protocols specific to your ICU. Consider keeping your protocols as simple and as visible as possible by placing them in convenient locations at the patients' bed-side so that they can be easily referred to when needed. For example, an enteral nutrition feeding algorithm may be laminated and posted at the head of each patients bed.
3. Identify Barriers to Feeding Patients (Click the thumbnail below to open a larger image)
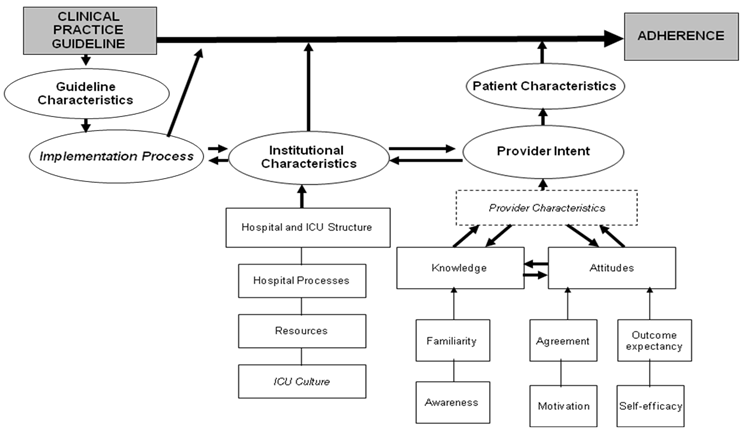
Sometimes there are barriers that hinder the implementation of nutrition guideline recommendations. Our research team conducted a qualitative study to understand barriers to adhering to nutrition guidelines and assimilated the results into a framework. The five barrier domains included in the framework were as follows:
- Guideline Characteristics: Guidelines consisting of complex statements that are difficult to interpret, or are based on outdated or weak evidence, are barriers to guideline adherence.
- Implementation Process: Lack of adequate resources in terms of time to plan, conduct and attend educational sessions are barriers to effective guideline implementation.
- Institutional Factors: Being a small, non-teaching hospital, in a rural location with an open ICU structure (i.e. any attending physician can admit to the ICU) are institutional characteristics that act as barriers to guideline adherence. Resource constraints (e.g. staff, materials, specialty services) and a slow administrative process are additional barriers. An ICU culture where there is no cohesive multi-disciplinary team structure, lack of leadership, and poor communication are also barriers.
- Provider Intent: A critical acre providers' intent to adhere to the guidelines is based on their knowledge of and attitudes towards the guidelines. Knowledge is a function of ones familiarity and awareness of the guideline recommendations. Attitude is a function of outcome expectancy (i.e. belief that following the recommendation will benefit the patient), self-efficacy (i.e. belief that one has the skills to implement the recommendation), motivation (i.e. the willingness to change) and agreement with the guideline recommendations. A providers' knowledge, attitudes and intent to adhere to the guidelines are further influenced by their profession (physicians vs. nurses vs. dietitians), educational background, critical care experience, and personality.
- Patient Characteristics: Guideline adherence is more difficult in patients with a poor prognosis or for whom there are other more urgent priorities of care.
Overcoming these barriers is crucial to changing nutrition practice. This highlights the importance of assessing local barriers to feeding patients and designing interventions to overcome these barriers. A barriers assessment may be in the form of a questionnaire, interview, or focus group with ICU staff, followed by a brainstorming session with key staff members to identify feasible solutions to the problem. We conducted a feasibility study, entitled the PERFECTIS Study, to provide preliminary evidence of the logistics and feasibility of identifying barriers to adherence to key recommendations of the Canadian Critical Care Nutrition CPGs and tailoring guideline implementation strategies to overcome the identified barriers and improve adherence. For more information on this study, click here.
In addition, our Barriers Questionnaire was recently revised in September 2013. Click here to learn more.
4.Improve Nutrition Knowledge
The delivery of nutrition is the responsibility of the multi-disciplinary team and not the dietitian alone. The role of the intensivist, non-ICU physician, critical care nurse, and other team members are essential, but fulfilling this role can be challenging particularly for practitioners who have not received any training in critical care nutrition.
The Resource Center provides numerous training materials and information documents to increase awareness of nutrition guidelines and improve knowledge of nutrition therapy among critical care providers. These training materials may be used in the context of formal and informal education such as:
- Presentation during grand rounds or in-services
- Bed-side instruction (one-on-one or small groups)
- Workshops
- Computer based learning modules
- Visual reminders (e.g. posters, screen shots)